- 1st January 2016 – a Day I Will Never Forget
I arrived at the station early in the afternoon to say goodbye to some of the army paramedics whom I’d become close to. They were leaving to finish their course in the army. I remember the MDA paramedics, we the volunteers, we were all just sitting around chatting and eating cake and waiting for our ambulance to arrive back from the morning shift.
At around 2:25pm, I heard over the loud speaker that Nathan Aleph (the evening ambulance I was to work on) would have to take out the spare ambulance. Usually, we take out an extra ambulance if the evening shift needs to start before the morning shift ambulance arrives back.
So I walk outside to the ambulance and I see Ronen, who did the morning shift. He says to me, “Quickly get to the ambulance”. I still didn’t know exactly what was going on, but I knew something had happened because about eight ambulances had left the station all at the same time.
In the ambulance, I asked my paramedic what had happened. He said that there had been a terrorist attack on Dizengoff Street – a shooting.
My heart jumped out of my skin. I was scared. I didn’t know what to do. I just followed each order. I was told to put on a bulletproof vest before we arrived at the scene. When we got to Dizengoff Street, I saw hundreds of police and people screaming in the streets. I still remember the sounds of the screams. I later found out that over 2,000 policemen had been called to the scene from all over the country.
 Usually when we get to calls, we don’t run. But in this situation, I was told to grab the bed from the ambulance and run. As I got closer to the scene, I saw blood everywhere – people lying on the floor, people screaming. We were the second ambulance to arrive at the scene. We went to the first patient we saw. There was already a medic performing CPR on the patient. The place was so tiny and there were so many people trying to help. We were all so squished, trying to help this patient. Usually when we get to calls, we don’t run. But in this situation, I was told to grab the bed from the ambulance and run. As I got closer to the scene, I saw blood everywhere – people lying on the floor, people screaming. We were the second ambulance to arrive at the scene. We went to the first patient we saw. There was already a medic performing CPR on the patient. The place was so tiny and there were so many people trying to help. We were all so squished, trying to help this patient.
I stepped outside of the Simta Bar for a moment and heard someone next to me screaming and crying out “Paramedic, paramedic, help my brother!”. I was shocked, I didn’t know what to do, I froze. The paramedic grabbed me and pulled me in with her back to help our patient. I knew that another ambulance was right behind us. They were going to be there any second and would help. I couldn’t believe how much blood there was everywhere I looked. We managed to get our patient onto the bed and ran with him to the ambulance. This was all in a matter of three minutes!
Running past everyone, I could still hear the screaming and the crying. In the ambulance, we were giving him CPR, trying to give him oxygen. However I knew that CPR in trauma is never a good outcome. It was such a rush. I can’t even remember what I was doing in the ambulance. Everything just happened so quickly.
We arrived at Ichilov hospital and the paramedic gave me the patient’s wallet to go and open a file, while they rushed him into the trauma room. I opened a medical file and looked at his name – it was Shimon. That’s all I could remember. I then went into the trauma room and there were around forty doctors and nurses standing and helping. I saw the doctor crack open his ribs to see if there was any internal bleeding. Once he had done that, he then called the CPR off. This man, our patient, had died from his internal wounds from the shooting.
I still had this man’s wallet in my hand, so I went outside to give it to his friend. At this point, I knew very well that he had died. I faced his friend and gave him his wallet. It was very difficult for me because I knew that his friend did not know the outcome yet. I felt terrible.
I walked outside of the hospital to help clean the ambulance and to take a deep breath and consider what had just happened. I was sitting in the back of the ambulance when I saw another ambulance arrive. I looked across and saw what I thought (and later found out to be) the mother and father) of another patient arriving. I saw the paramedics take this patient out of the ambulance. He was connected to a device called a “Lucas”, which gives automatic compressions.
I looked across at the parents and saw the father faint and the mother scream. This was probably one of the worst sights I’ve ever seen. It was later released that the patient with the “Lucas” attached was Alon, the manager of the Simta Bar.
After a while, we were still at the hospital, waiting to see if they needed us to go back to the scene to pick up any other patients. The paramedics asked me if I knew the name of our patient. I said that I thought his name was Shimon. A couple hours later, it was released, in the news, that a second patient had died and his name was Shimon. We knew that he was our patient. Three people died from this attack that day, and one of them was our patient.
To this day I don’t like to talk about it.I just remember the vivid images and the scenes of that day. I think that the best way to describe my feelings were just numb and scared.

MDA personnel were on the scene within minutes. It just proves to me what an important organisation it really is. Everyone worked so hard together that day and I believe we became closer to each other after such a traumatic experience.
- December 2015 – a Prostitute, Football and Jerry Seinfeld
I’m now up to week five of volunteering in Israel and I’m enjoying my time in MDA more than ever. It’s started to get easier to wake up at 5:45 am as now my body is very used to the routine.
On this particular call, we were called to the Tachanat Merkazit (Central Bus Station). We were told that the person was having trouble breathing. As we approached our destination, we were greeted with a very friendly, over-excited patient. She was 40 years of age. She came straight up to the ambulance window and announced that she had AIDS, hepatitis B and she thinks she may also have had tuberculosis.
She entered our ambulance and we checked all her vitals. She had an increased heart rate – other than this she was okay. She wanted to go to the hospital, so we took her. She mentioned to us that she had taken a few drugs that day too. On the way to the hospital, she proceeded to tell us that she’d left home at a very young age and had became a prostitute. When she was diagnosed with AIDS, she then stopped and is now homeless, living on the street. She was a very interesting patient to listen to and to hear her story.
On another morning, I was very lucky to be working with a well-known actress and journalist in Israel – Yamit Sol. During her busy schedule, she takes time to volunteer for MDA.
 Our first call of that morning was to a man who had been running in Yarkon Park and had collapsed. When we arrived, there was nowhere close to the scene where we could stop the ambulance. So the paramedic, Yamit and I took all the equipment and walked across the park to the man on the ground. People were already surrounding him and had began CPR. When we came, the paramedic intubated him and we gave him all the medications he required. Unfortunately, this man didn’t survive. Later, we found out that he was the chairman of a major sports company in Israel. Our first call of that morning was to a man who had been running in Yarkon Park and had collapsed. When we arrived, there was nowhere close to the scene where we could stop the ambulance. So the paramedic, Yamit and I took all the equipment and walked across the park to the man on the ground. People were already surrounding him and had began CPR. When we came, the paramedic intubated him and we gave him all the medications he required. Unfortunately, this man didn’t survive. Later, we found out that he was the chairman of a major sports company in Israel.
 A week later, I attended the soccer to watch Maccabi Tel Aviv play Beer Sheva, their major rival. At the beginning of the match, the ground announcer spoke about this man and about his life. It was a weird feeling to know that I was one of the people to provide him with medical treatment. A week later, I attended the soccer to watch Maccabi Tel Aviv play Beer Sheva, their major rival. At the beginning of the match, the ground announcer spoke about this man and about his life. It was a weird feeling to know that I was one of the people to provide him with medical treatment.
Jerry Seinfeld was performing his shows in Israel. I was very excited to attend one of them with the ambulance. MDA is present at all types of events in case something happens. During the intermission I was walking around. Suddenly, people began screaming for MDA to come. I ran to the scene where a security guard was in the middle of a seizure. We treated him and then sent him off to hospital. After this, we were able to watch the show. Jerry was absolutely hilarious – I couldn’t stop laughing the entire time. This was one of the most enjoyable events I’ve attended and been a part of during my volunteering in Israel.
- December 2015 – Another Week Gone by
It’s always an eventful week when it comes to working in MDA. We constantly have calls to sick patients and some of the most common calls involve chest pain, trouble breathing and seizures. On the odd occasion, we’ll get something quite different or more intense.
 This particular call to a patient with shortness of breath was something quite different. In fact, when we arrived at the home, we found not only the old man suffering, but his wife also. They were both having difficulty breathing. We treated them both at the same time by checking their oxygen saturation levels, checking their heart rate and their blood pressure levels. We then called another ambulance to help evacuate one of the patients. On the way to the hospital, we called the emergency department to make space for two patients, so they could have a “suite” together in the hospital. They very much appreciated that. This particular call to a patient with shortness of breath was something quite different. In fact, when we arrived at the home, we found not only the old man suffering, but his wife also. They were both having difficulty breathing. We treated them both at the same time by checking their oxygen saturation levels, checking their heart rate and their blood pressure levels. We then called another ambulance to help evacuate one of the patients. On the way to the hospital, we called the emergency department to make space for two patients, so they could have a “suite” together in the hospital. They very much appreciated that.
During another shift, we were having fun, singing songs in the ambulance. A call to a 20 year old girl came in. Her roommate had arrived home to find her hanging from the bathroom door. He had cut her down and, by the time we arrived, there were other medics who had arrived on motorbikes. We began giving her CPR.
 It was very challenging to see this as she was so close to my own age. She had rope marks around her neck. In the coming weeks, she had been scheduled to start hormone treatment to become a man. She also had a history of depression. It was very challenging to see this as she was so close to my own age. She had rope marks around her neck. In the coming weeks, she had been scheduled to start hormone treatment to become a man. She also had a history of depression.
During the CPR, I was instructed to give her breaths every six second, using the ambu-pump. There were six other men and they were instructed to switch between giving compressions. After around 45 minutes, we were unable to revive her and the paramedic pronounced her dead. This was a very tough call to be a part of. I thought that maybe we had got to her in time, but unfortunately we didn’t.
 The next call came in almost immediately after this. It was to a man who, we were told, was suffering from hypoglycaemia. When we arrived, he had a pulse, but was non-responsive to pain, or anything else. Yaarit, the paramedic, intubated him and, again, I helped with providing him with oxygen. We managed to get him into the ambulance and, on the way to the hospital, we noticed that his vital signs were dropping – fast! We checked his blood pressure – 40/20. Around 120/80 is normal. While our driver, Barak, was speeding towards the hospital, Yaarit began compressions. I’ve never seen someone’s vitals drop so quickly, and so suddenly. When we arrived at the hospital, we rushed him into the trauma room, where the nurses and doctors connected him to a device called the “Lucas” – an automated compression pump. The next call came in almost immediately after this. It was to a man who, we were told, was suffering from hypoglycaemia. When we arrived, he had a pulse, but was non-responsive to pain, or anything else. Yaarit, the paramedic, intubated him and, again, I helped with providing him with oxygen. We managed to get him into the ambulance and, on the way to the hospital, we noticed that his vital signs were dropping – fast! We checked his blood pressure – 40/20. Around 120/80 is normal. While our driver, Barak, was speeding towards the hospital, Yaarit began compressions. I’ve never seen someone’s vitals drop so quickly, and so suddenly. When we arrived at the hospital, we rushed him into the trauma room, where the nurses and doctors connected him to a device called the “Lucas” – an automated compression pump.
Unfortunately, the patient did not make it. This was a major shock to the family, as they didn’t realise how bad the situation was. Initially, after they had called for an ambulance, they then cancelled the call – only to call back 10 minutes later. I really understood how every second can save a life.
There was another memorable call as it was something I’ve never before experienced. We were told that the patient had had an accident, however we weren’t given many details. We arrived at the scene and the paramedic called out to me to bring him the back-board and a neck brace. When I got close to the situation, I saw that there was blood everywhere. His hair line had been ripped off and I could see a large amount of his skull. We quickly put bandages around his head to stop the bleeding and then back boarded him into the ambulance. When we tried to take his blood pressure, he screamed in pain. This indicated that he had most likely also broken his arm.
On the way to the hospital, we were trying to stabilise his head. I couldn’t believe how much blood there was. It was running through the entire ambulance. We had to put sheets down everywhere to stop it from going into the front driver’s seat. The paramedic told me that he had fallen off a four-wheeled bike. He hadn’t worn a helmet or any other protection. A CT scan later showed that he had also broken many bones in his face.

Another week gone by…
If I thought the first week wasn’t busy enough, this week was probably the most intense week I’ve had out of all my time volunteering for Magen David Adom.
I was doing a shift with my friends Mostfa and Shai. We were at the station checking the ambulance when we get a call to a 71 year old unconscious man in a parking lot. We arrive on the scene. T Lavan team was already there, performing CPR on the patient in the ambulance. We needed more room so we could intubate the patient and start a line (to inject adrenaline and other necessary medication). So we took the patient out of the ambulance and into the parking lot. I looked around – there were people everywhere, watching, their eyes gazing at us, some in complete distress, others curious to see what was going on.
We had lots of medics helping. I was helping with the compressions as well as with the oxygen. We managed to get a small pulse, so we quickly put the patient into our ambulance, the Natan, and rushed him to the hospital. In the ambulance, I kept giving him the oxygen, however, when we arrived to the hospital, the man lost his pulse. A but sherut who was helping us had to sit on the patient and manually give him compressions, while we rushed him into the intensive care unit. Unfortunately, the patient did not survive.
We were tired after the long call and, once all the paperwork was done, we were available for more calls and on our way back to the station.
We then heard our ambulance being called on the radio to a lady in a car on the highway. She was having trouble breathing, so we put on the sirens and we were on our way. We were then informed that the 57 year old lady was now unconscious in the car with her two friends.
My initial thoughts were, “Oh no, another CPR!”. This is because it is very labour intensive and can go on for hours. When we arrived, we blocked off two lanes of the highway and the adrenaline kicked in. No longer was I tired, but I was ready to try and help to save this woman’s life.
She was in the front passenger seat of the car. Mostfa carried the woman out of the car so we could intubate her and start a line. Her friends were extremely distressed and asked me “What do we tell her husband?”. I replied that they should tell him what had happened and Ichilov hospital. I wasn’t sure if this was the right answer -but I wasn’t sure what else to say. I immediately took the cardio pump and began the compressions. As I’m counting, I can hear cars driving past and honking their horns. I couldn’t believe the situation we were in. Giving CPR in the middle of a busy highway.
As I was giving compressions, the woman was vomiting everywhere. The paramedic was trying to intubate her, but there was so much vomit everywhere and it went all over us all. We had to keep going – we couldn’t stop. This woman was so young. We needed to intubate her and start a line. We also shocked her in order to start a new heart rhythm.
We got a pulse and again we were off to the hospital. In the ambulance, the patient was stable and I was giving her oxygen. When we arrived at the hospital, the doctors couldn’t believe we had another CPR. This patient remained stable, however I’m not sure about any potential brain damage to this patient.
These two calls took up majority of our eight-hour shift. When we finished, we were all exhausted and ready to go home to sleep.
The next morning, with my friend Moshiko, I did a shift at the Ramat Gan station which is MDA Australia-sponsored. With us were also Dudu (the paramedic) and Adi (a trainee paramedic). This shift was pretty quiet the whole time. We were sitting and chatting, and not much went on during the shift. We only had one call to a patient who had difficulty breathing.
I needed to get back to Tel Aviv after the shift, so an ambulance driver who had just finished his shift was available to take me. I jumped into the ambulance. We were sitting in heavy traffic, nearly at the Azrieli mall, when we hear our ambulance on the radio. We were confused, but answered the “moked”, who told us we must go to the call.
The call was to a man who had committed suicide and had jumped off a roof. So we turned the ambulance around and the sirens went on. When we arrived at the scene, we were one of the first ambulances there and the police were everywhere. I saw the man lying on the ground with blood everywhere. There was nothing we could do. We needed the paramedics to arrive in order to pronounce the man dead. It was a horrible scene. An image I unfortunately will never forget. We were able to leave the scene once the paramedics arrived. The man had been pronounced dead.
As if I thought this week couldn’t get any more intense! The next day, I was working with Ronen. A call came in to another unconscious man, 44 years old. Israel has many people from Asia who are employed to look after the elderly. Usually, it is these helpers who call to say that the person they are looking after is unwell. This was different. This was an elderly man who had called MDA for his carer who was unconscious.
The man had passed out in the bathroom. We took him into the living room. I was helping with the compressions and organising medication for the patient. The paramedic intubated him and we got a pulse back. When we perform CPR on a patient, it may seem as if it takes 10 minutes. However, we can be giving them compressions for an hour before we get a stable pulse back. We took the patient to the hospital with a stable pulse and he survived, however I’m not sure what type of damage he incurred. After the call I asked Ronen what may have happened to him. He said that it could have been an issue with the heart or the brain.
That was just the first half of my week! Luckily, the rest of the week was not as intense as this. I had lots of calls to patients with chest pain, where I was able to perform an ECG on them. Also, we had a few patients with COPD – we gave them an inhalation.
I’m starting my third week with MDA. I wonder what that has in store for me!
And… I’M BACK!!! Can you tell I love volunteering for MDA in Israel? It’s so good to be back.
My first week in Israel was exciting. Glynis and I ordered a Young MDA Victoria motorcycle. The first major purchase that I was involved in. What a feeling!
After my first week in Israel, it was time to begin volunteering on the ambulances – I couldn’t wait! Every time I heard a siren I’d turn around, hoping to see an MDA ambulance, hoping that I’d catch a glimpse one of my friends in the window.
 My first shift (no surprise here) was with Ronen. There is a running joke at the station that I’m Ronen’s personal “mitnadevit” (volunteer). This is because I love working with him and I always work with him. I understand the way he works and I always know his next step. This makes for a really good team and that’s what we are. My first shift (no surprise here) was with Ronen. There is a running joke at the station that I’m Ronen’s personal “mitnadevit” (volunteer). This is because I love working with him and I always work with him. I understand the way he works and I always know his next step. This makes for a really good team and that’s what we are.
This shift was a busy one. We were constantly on the go. The first call, on my return, was to a lady having an asthma attack. We gave her the necessary medication and I put on her an oxygen mask. We then took her to a hospital I’ve never even heard of, called Mayer. The rest of the shift we took people to Ichilov hospital all with chest pain.
 The next day, I decided to do a double shift. I did a morning shift and then stayed on to do an evening shift with my other friends – Oz, Mostfa and Liza (a new paramedic). This was really a fun shift and, while we weren’t on any calls, we were all having fun and enjoying each others’ company. The next day, I decided to do a double shift. I did a morning shift and then stayed on to do an evening shift with my other friends – Oz, Mostfa and Liza (a new paramedic). This was really a fun shift and, while we weren’t on any calls, we were all having fun and enjoying each others’ company.
The first call was to unconscious baby, not breathing. We were prepared for the call and had read through the protocols of what to do on an occasion like this. When we arrived (it was on the street), we could see the baby kicking and screaming so that we knew straight away that it was a good sign. We checked the baby’s vitals and I held her in the ambulance while the paramedics treated her. It seemed as if she was in post-seizure, which likely had something to do with temperature. The baby was so adorable with her big blue eyes. We took her to the children’s department at Ichilov hospital for further tests.
Another memorable call was to a woman who had fainted in the “tachanat merkazit” (central bus station). Initially, she wasn’t talking. We didn’t know her name and she didn’t want our help for anything. She was refusing all treatment. We tried to test her blood pressure and sugar levels, however she kept refusing for about 45 minutes. The paramedic then called the doctor who gave us permission to leave the call.
After this double shift I was exhausted. I couldn’t wait to go home and get into bed.
The next morning, I was up bright and early again for a morning shift, this time on the “lavan” (white ambulance) with Mostfa and a “bat sherut”, Audelia, with whom I’d become friendly last year. We also had another volunteer, Jill from America. It’s a deal that I have with Mostfa, that if we work together on a morning shift, he’ll take us for hummus for breakfast (if we have time). That’s exactly what we did and it was so delicious! We had a fun day singing songs on the ambulance, while we had no calls – just all hanging out.
We had a few calls that day which included a young girl who had appendicitis. Another call was to a man who had just fainted. All of these calls, we checked their vital signs and then took them to the hospital.
On that day, while on the way hospital, we heard on the radio that there had been a “pigooah” (terrorist attack) in the south of Tel Aviv. When we arrived at the hospital, there were paparazzi and news reporters everywhere. There was so much security everywhere. One of the ambulances at the hospital was covered in blood. When I went inside the hospital I saw a glimpse of a body laying on the table in the trauma room. This man had a small pulse when the paramedics had got to him but, unfortunately, had died of his wounds in the hospital.
 Later, our ambulance was called to the site of the “pigooah”, to a lady suffering from stress and anxiety from what had happened. We arrived at the scene but the call was then cancelled. Later, our ambulance was called to the site of the “pigooah”, to a lady suffering from stress and anxiety from what had happened. We arrived at the scene but the call was then cancelled.
My first week was incredible, seeing my friends and being involved in the life-saving work of Magen David Adom. I’m so happy to be back.
Stay tuned…
Some of the most intense calls that I attended were very confronting, simply because these were things I’d never seen before. Three such calls that come to mind.
The first call to a man on the street having chest pain. When we arrived, the paramedics jumped out and ran over to him. They then screamed, “Julia, bring the stretcher quickly!”. I jumped out, took the stretcher over to them and, in a matter of 15 seconds, the man was on the stretcher and in the ambulance. The paramedics work so fast it is sometimes hard to keep up with what they’re doing. But you get used to it – you have to. At this stage, I wasn’t entirely sure what was going on with the patient. I could just tell something wasn’t right. As soon as the paramedic shaved the man’s chest and put the defibrillator pads on, I knew he was having a heart attack. While my mind was racing at a million miles per hour, I was preparing all the medication for the paramedics – syringes, needles, bandages, gauze pads, saline solution, oxygen and the rest.
 We were prepared for the worse. When we arrived Ichilov hospital we didn’t go to emergency, but straight to the cardiovascular department. We raced the man up in the elevator straight into surgery where the surgeons were already waiting for him. At this stage, the man was doing okay, but was clearly still struggling. We were prepared for the worse. When we arrived Ichilov hospital we didn’t go to emergency, but straight to the cardiovascular department. We raced the man up in the elevator straight into surgery where the surgeons were already waiting for him. At this stage, the man was doing okay, but was clearly still struggling.
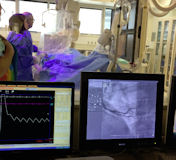 The doctors then took over and we explained to them what had happened and where we’d picked him up. I then went behind the glass to watch the surgery from the viewing room. I saw the surgeons cut open the femoral vein in his thigh and proceeded to insert a stent to his heart. This took 10 minutes, following which the man was placed into intensive care. The doctors then took over and we explained to them what had happened and where we’d picked him up. I then went behind the glass to watch the surgery from the viewing room. I saw the surgeons cut open the femoral vein in his thigh and proceeded to insert a stent to his heart. This took 10 minutes, following which the man was placed into intensive care.
Another call which stands out was very emotional me. I walked into an office building where a man was hanging from the ceiling. That image will never leave my mind. But it just shows that, on an ambulance, you see everything. MDA workers are so professional, I really admire how they apply themselves to their daily tasks.
Then there was that difficult night. It was 10:25pm and we’d almost finished our shift. Just as we approached the Tel Aviv station, our ambulance was called over the radio to attend a stabbing. It was right next to the Central Bus Station, where a man had been robbed and stabbed in the back of the head. Again, in these types of calls, we need to work extremely fast. Within 15 seconds, we had him in the back of the ambulance. Immediately, the two paramedics with whom I was working were opening veins to insert saline and the other necessary drugs. I was putting a compression bandage around his head to stop the blood flow. We rushed him to the emergency department in Ichilov and passed him onto the emergency doctors to continue with his care.
 Even though I had these intense calls, on a few occasions I was lucky enough to be selected to go on the ambulance attending Maccabi Tel Aviv soccer matches. I would arrive to the station at 5:30pm and head off in the ambulance to Bloomfield Stadium. I also had the opportunity to sit on the sidelines with the stretcher. It was so incredibly exciting and loud – and I loved it! Even though I had these intense calls, on a few occasions I was lucky enough to be selected to go on the ambulance attending Maccabi Tel Aviv soccer matches. I would arrive to the station at 5:30pm and head off in the ambulance to Bloomfield Stadium. I also had the opportunity to sit on the sidelines with the stretcher. It was so incredibly exciting and loud – and I loved it!
 This has definitely been the best experience of my life. I thought that I made lots of friends in MDA when I volunteered the last time. But, this time, not only did I get to see my old friends, but I made many more new ones. I can’t wait to go back to see them all! This has definitely been the best experience of my life. I thought that I made lots of friends in MDA when I volunteered the last time. But, this time, not only did I get to see my old friends, but I made many more new ones. I can’t wait to go back to see them all!
- Wednesday, 7th January 2015
What a busy few weeks it has been! Many calls we receive are shortness of breath, trouble breathing and chest pain.
While working the other day, my ambulance received a call to go to a construction site in Ramat Gan because a metal bar had fallen on a worker. When we arrived, we walked over to the site which was 5 metres below the ground – they were in the middle of building an underground car-park for the residents. We were greeted by three fire trucks and another ambulance which had already begun helping the man.
I was looking from above the site, watching the firemen wrap the man up in a special type of backboard, which connects to the fire truck, in order to lift the man out of the construction site. Once lifted out of the ground, we went over to the man and put him in our ambulance. We needed to be very careful as we were unsure, at that stage, of what injuries he may have acquired.
Once in our ambulance, we checked his vital signs and asked him about where his pain was. He told us that the bar had fallen on his head and he also had a really bad pain in his left knee. We arrived at Ichilov Hospital, where the paramedics told the guards that our patient was not from Israel (unbeknown to me). The paramedics told me that he was from Gaza and was working in Israel on a special visa.
Another interesting that case I recently had was at the Central Bus Station (Tachanah Mercazit) at 11:00 am. We had picked up an American man, who had been living in Israel for 25 years, who had told us that ten black men had beaten him up at 3:00 am. We asked him what he was doing at the bus station at 3:00 am. He told us that he was picking up his ID which he left there. He spoke a little bit of Hebrew, but mainly English – so we spoke to him in English.
His story was that some guy pushed him. So he turned around and pushed him back. Then another nine people came and started attacking him. He incurred a black eye and a cut on his head during this ordeal. According to the paramedic, he told me that this story did not seem right at all and the most common reason to be at the bus station at 3:00 am was because he was looking for drugs or for a prostitute. We took him to Ichilov, where the nurses and doctors placed him under observation for a few hours.
- Monday, 8th December 2014
 Everyday is a routine – I wake up to be at work at 7:00am, get on an ambulance and then the three or four of us, who are on that ambulance, check the ambulance together. We check the oxygen, we check that we have a certain amount of each medication, a certain amount of needles and syringes and birth kits. We check that all the equipment is working, such as the monitor, as well as many other things. Everyday is a routine – I wake up to be at work at 7:00am, get on an ambulance and then the three or four of us, who are on that ambulance, check the ambulance together. We check the oxygen, we check that we have a certain amount of each medication, a certain amount of needles and syringes and birth kits. We check that all the equipment is working, such as the monitor, as well as many other things.
Over the past few days I have had some very interesting cases.
My Intensive Care (MICU) ambulance received a call that a baby had had a seizure. When we arrived at the scene, the baby was crying with tears, which immediately gave us the positive sign showing that she was conscious. We took the baby and the grandmother to hospital and, on the way, we were able to check the baby’s vital signs, which were all okay. Once at the hospital, the nurse took the baby’s temperature and confirmed a high temperature of 38.5oC degrees. Ronen and Yaarit, the paramedics with me that day, explained that the seizure was connected to a fever and that this was because the body was unable to release the heat. The baby was taken care of at the children’s hospital in Tel Aviv.
Another fascinating call I attended was to a “junkie site” for a heroin overdose. We arrived in an area known for drugs and prostitution. We found the man on the ground, surrounded by syringes. He had a small pulse of 4 breaths per minute and was unresponsive. Immediately, we began ventilating him and helping him to breathe. Meanwhile, Ronen and Na’ama (both paramedics) worked on getting a line into his arm in order to give him the medication he needed. After 10 minutes, his oxygen levels increased, as did his pulse. He began to become conscious again. When he woke, we told him that we are MDA and were there to help. He sat up and vomited everywhere. However he didn’t want to come to the hospital with us. We made sure he was okay and then left the site.
The first call of my day, today, was to an unconscious man. We arrived at the scene to see an old man, not breathing and unresponsive. We began CPR. Ronen and Oz (paramedics) worked on clearing his airway and putting a tube into his lungs so that oxygen could travel to the rest of his body. We used the cardio pump to manually pump his heart in order for his blood to circulate. After what seemed like forever, we were able to get a pulse. However, the man was still unconscious and unresponsive. We took him to the hospital where the doctors scanned his brain and his body. Unfortunately, this man was brain-dead, so that there was not much else to do except for the doctors to inform the family.
 However, not all calls we receive are upsetting. This one was, in fact, very exciting and amazing – a birth!!!! After a total of four months working for MDA so far (in 2011 & 2014), I arrived to see my first birth! The partner of the woman had delivered the baby before we arrived, but it was up to us to cut the umbilical cord and check the vital signs of the mother and the newborn. All signs were good, so we took mother and baby to the hospital, where the doctors removed the placenta and washed the baby. While in the ambulance, I was asked to hold the newborn – it was such a beautiful feeling!! However, not all calls we receive are upsetting. This one was, in fact, very exciting and amazing – a birth!!!! After a total of four months working for MDA so far (in 2011 & 2014), I arrived to see my first birth! The partner of the woman had delivered the baby before we arrived, but it was up to us to cut the umbilical cord and check the vital signs of the mother and the newborn. All signs were good, so we took mother and baby to the hospital, where the doctors removed the placenta and washed the baby. While in the ambulance, I was asked to hold the newborn – it was such a beautiful feeling!!
Back to reality – we received another call of an overdose in the same “junkie site” as the day before. This man was clearly struggling and wouldn’t let us put a drip in his arm. He was having trouble breathing, so we put an oxygen mask on him while we took him to the hospital. I noticed a protrusion on the right side of his chest, which looked like a pacemaker. When we were at the hospital, I found out that this man had been a soldier many years ago and had been injured in the Dolphinarium suicide bombing. As a result, he had received a pacemaker for his heart. As a response to what this soldier had been through, he turned to drugs.
I will continue to update you all on my MDA adventure. Please continue to donate to support the vital work of Magen David Adom.
- Tuesday, 25th November 2014
Three years on and I’m so excited to be back volunteering for Magen David Adom in Tel Aviv!
 I was lucky enough to work with Ronen Cohen, a favourite paramedic of mine. I’ve known for years and he has the patience to mentor me through all the cases, and teach me Hebrew at the same time. He is a dedicated paramedic who’s been working with MDA for over 30 years. He is well respected and loved by everyone including the overseas volunteers. I was lucky enough to work with Ronen Cohen, a favourite paramedic of mine. I’ve known for years and he has the patience to mentor me through all the cases, and teach me Hebrew at the same time. He is a dedicated paramedic who’s been working with MDA for over 30 years. He is well respected and loved by everyone including the overseas volunteers.
What an eventful first day!
I was stationed on an MICU in old Jaffa, however we didn’t make it to the station once as we were jam-packed with calls for the entire shift. The calls today included patients suffering from chest pain, high blood pressure or unconsciousness. All patients were transported to Ichilov Hospital in Tel Aviv.
My next shift is tomorrow at 7:00am on the MICU.
- Thursday, 8th December 2011
As of yesterday, I officially ended my MDA program. But I knew from the time I started the program, that one month was not going to be enough for me. So I extended my 6-month trip by another month in order to continue working for MDA.
I’d previously been volunteering in Tel Aviv, which I loved. I made great friends and met the most awesome Paramedics who constantly taught me new things every day. But, it was time for a change – a new region, where I could meet new people and experience new things. So, I packed up and moved to Jerusalem.
The most memorable cases that I’ve experienced were obviously those involving CPR. But, unfortunately, we couldn’t revive any of the patients. They were all over 70 and had different health problems which contributed to their deaths.
One woman we attended to had been unconscious for 3 hours. She was extremely pale and had a locked jaw. There was nothing that we could do for her because, once the jaw is locked, it becomes apparent that the person has not been conscious for a while and CPR must be started as soon as possible.
One unforgettable call which we received was to a 23 year old girl who was having seizures. We arrived on the scene, which was a youth hostel, the girl was on the floor shaking and being held down by four men. Initially, I thought it was so strange because I remember being taught in my course that if someone is having a seizure then you shouldn’t touch them. The paramedic then advised me that it wasn’t a seizure – she was actually having full-body muscle-spasms. So, once the spasms had stopped, we were able to talk to her. But she wouldn’t look or talk to any of the men who were ther. She would only talk to me – and she spoke like a 10-year-old girl – with an extremely high-pitched voice and only in Hebrew.
During this time, one of the male paramedics tried to put the Sp-02 clip on her to check the blood pressure in her brain. But she was resisting. She wouldn’t even let him touch her. I also tried. Even though she allowed me to touch her, she wasn’t allowing me to put the clip on her finger. I put it on myself and said, “Look” – to show her that it wasn’t going to hurt her. But she was still resisting.
While this was going on, Ronen (a paramedic and a close friend of mine with whom I worked nearly every shift) was on the phone to the young girl’s friend. The first thing that the young girl said to me that I could understand was “phone”. She lifted up her arms and, with her hands, took the phone with majority of her body crippled and stiff. After speaking to her friend for a few moments, she then handed me the phone. Ronen and I looked at each other. Ronen then explained to her that I don’t understand enough Hebrew to talk on the phone (I really wished that I’d learnt more Hebrew at this point). He took the phone and then, for the first time, the girl spoke to Ronen – still in a high-pitched tone.
She told him things to tell me and what to do for her because she wouldn’t let any of them men touch her. She explained to Ronen that I needed to shake her wrists and also rub her knees to relax her muscles in order for her to move. After I had done, this she was able to sit up. From them on, she spoke to Ronen in a normal- pitched tone and explained the situation to him. Unfortunately, I was unable to understand the majority of the situation and what was going on with her as she wasn’t speaking English. But then right when we were leaving, she shook my hand and said “Nice to meet you”. I asked her “Do you speak English?”. She replied “Yes”. I was amazed, because she wouldn’t respond to me when I had spoke to her in English initially. She told Ronen that she didn’t want to go to the hospital. So we made sure that she was ok and then left the scene.
In the ambulance, we filled out all the paperwork and I asked Ronen what was going on with her. He told me that he was devastated for her. I was confused, I had no idea what was going on. Ronen explained to me her situation. He said that when she was 12 years old, she had been raped. So, in order to deal with this, she’d developed a new personality within herself. This is called “Multiple Personality Disorder”. This personality that she’d developed was the 12-year-old girl who was raped and not the 23- year-old woman she was now.
She doesn’t believe that she is Sarah who’d been raped. She believes that this 12-year-old girl inside her (Duval) was raped. When she becomes “Duval”, and I don’t know how this happens, she starts to muscle spasm. When she had initially spoken to me about the reason why she spoke in such a high-pitched voice, it was because she was acting as Duval and she didn’t understand English because she was a young girl. She also wouldn’t let the men touch her because she was afraid of the men and thought that they would do something terrible to her. She was such a nice girl and we all felt terrible that she was in such a bad situation.
What went on that day all made sense to me when I was sitting in the ambulance listening to Ronen explain it to me. I thought that was the most confusing/interesting call I have had up until now.
I’ve been involved with Magen David Adom for the last 5 years. In 2008, I became President of Magen David Adom Teens (MDAT) and learnt about the MDA Ambulance Volunteer Program.
In 2010, I finished high school and decided to finish my gap year on the Volunteer Program. My training course started on October 24. The night before, when I attended the opening of the new Bloomberg Jerusalem MDA station, I met Reut, the co-ordinator of the Volunteer Program. I knew that I was going to enjoy it and learn so much from the program through her leadership and guidance. The course was going to be intense.
In MDA, you need to be tough, have confidence in yourself and in your ability to help and save lives. I knew, I could do it.
The first two things which we learnt were to be confident in your ability to learn to save lives and to be punctual. Wasting even one minute in a real-life situation can mean life or death. Our classes and activities ended at 8:00pm, but we continued to study, as well as learning Hebrew which consisted of hundreds of medical terms. I did this for 10 days straight!
The social aspect of the course was incredible. We were all there for the same reason – to save lives. We all shared the same experience of physical and mental drain. Our instructors were friendly, fun and exciting and had different ways to help us learn. We even learnt a dance to help remember part of PHTLS (Pre-Hospital Trauma Life Support).
The course included basic CPR on children, infants and adults, back- boarding a trauma patient and cleaning up blood on patients. Everyone was always willing to help one another and learn because we didn’t have to be there, we chose to be there.
I really enjoyed the learning aspect. On completion, we had a written exam as well as three practical exams which included back- boarding, CPR and bandaging. It was essential to make an effort as not everyone passed the first time.
I have had ten shifts so far. There have been two special ambulance call outs.
The first was the last call on my first day. We were called for “back up” because the medics had trouble lifting an obese woman up her stairs as she didn’t fit into the elevator. Our ambulance was the second one to arrive and we ended up calling another three ambulances. It took an hour and a half – and twelve sweaty men – to finally get her to her first floor apartment.
The second call was while I was working on the Natan (MICU). When we arrived, an unconscious man was sitting on his couch in front of the TV with his eyes open. He was not breathing and had no pulse. We immediately started CPR. There were four of us. I used the cardio pump and the senior medic inserted an IV into the patient’s arm. The medic put the airway into the patient’s mouth. During the compressions, I used all my weight every single time I pressed up and down on the patient to get his heart working again. After five rounds of thrity compressions, I was exhausted, so we switched around. We continued with CPR for thirty minutes with no results.
Unfortunately the patient did not survive. He suffered from diabetes, heart problems and was mentally ill.
Even though disastrous events can occur, being in Israel and volunteering for MDA has made me realize how much MDA truly does mean to me and what an incredible organisation Magen David Adom really is!
|
 Julia Caplan
Julia Caplan Julia Caplan
Julia Caplan